The Differences between Minimally Invasive Surgery and Traditional Surgery
Introduction of minimally invasive surgery
Many patients believe that minimally invasive surgery is simply surgery with small incisions. While it is true that minimally invasive surgery has smaller incisions, whether a surgery is minimally invasive or not is not determined by the size of the incision, but by the extent of damage to important tissues while ensuring the effectiveness of the surgery. If the focus is solely on minimizing the incision, the field of view may not be clear, exposure may be insufficient, and there may be stretching, injury, or compression to important tissues. This can lead to missed lesions, inadequate treatment and even if the incision is small, it cannot be considered minimally invasive surgery. Therefore, only surgery that minimizes both the "form" (small incision) and the "substance" (important tissues), is considered minimally invasive surgery and is the standard for surgical minimization.
For example, the reason lumbar disc herniation endoscopy surgery is regarded as a minimally invasive surgery is not just because of the small incision, but because every step of the surgery has been minimized.
Key to achieving minimally invasive surgery is the surgical approach. Through this path that passes through the skin, muscle, intervertebral foramen, and spinal canal, a passage is established that allows the endoscope to access the protruding intervertebral disc and nerves to remove the protrusion and release the nerve root. Minimization is reflected in the following aspects.
The difference between minimally invasive surgery and traditional surgery
Small skin incision: it is only about 0.5 cm, much smaller than the 8-10 cm incision of traditional surgery.
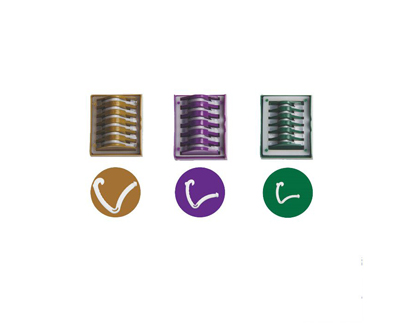
Less damage to muscles: during surgery, the muscle tissue is gradually expanded by a series of dilators, and muscle fibers are bluntly separated to create a cavity, instead of being cut with an electric knife or separated from the bone by peeling the periosteum, thus causing less blood loss and faster healing after surgery. It has no effect on muscle contraction strength and muscle content, and does not cause postoperative muscle pain or adhesions, nor does it cause stiffness or inflexibility in the back due to scar healing of the back muscles.
Less damage to bones: both traditional surgery and endoscopic surgery require access to the spinal canal. The former is achieved by cutting part or all of the vertebral plate, spinous process, and zygapophyseal joint, which "breaks the wall" from the side or back of the spinal canal, inevitably causing damage to the spinal structure, and making spinal instability difficult to avoid. Therefore, fusion fixation is required. Minimally invasive surgery, on the other hand, "jumps" into the spinal canal through the body's own natural opening - the intervertebral foramen - in order to conveniently access the working channel in the spinal canal and remove the protruding intervertebral disc. It may be necessary to moderately enlarge the window, which involves removing a part of the upper zygapophyseal joint by using a circular drill or saw to grind down the bone tissue of the intervertebral foramen. However, this part is actually very small, only 2-3mm, and the circular drill only grinds the ventral side of the facet joints, which has almost no effect on the joint surface, let alone the joint capsule on the back, and there is no impact on the movement and stability of the lumbar facet joint.