Efficacy Of Balloon Uterine Stent
1 Materials and methods
1.1 General information
A total of 70 patients with intrauterine adhesions admitted to our hospital from October 2013 to October 2014 were selected. All patients were diagnosed by hysteroscopy and had no abnormal leucorrhea, endocrine and breast function. According to the random number table method, the patients were divided into the study group and the control group. Among them, there were 35 cases in the study group, aged 23-45 years, with an average age of (31.4±1.5) years old, 1-5 times of pregnancy, and an average of (2.6±1.5) years of pregnancy. 0.3) times, uterine cavity operation times 1-5 times, average (2.3±0.9) times; control group of 35 cases, aged 22-45 years old, average age is (31.2±0.9) years old, pregnancy times 1-5 times, average Pregnancy times (2.5±0.6) times, uterine cavity operation times 1-5 times, average (2.4±0.5) times, there was no significant difference in age, pregnancy times and uterine cavity operation times between the two groups (P>0.05). For comparability, the study was approved by the ethics committee, and all patients gave informed consent and signed an informed consent form.
1.2 Methods
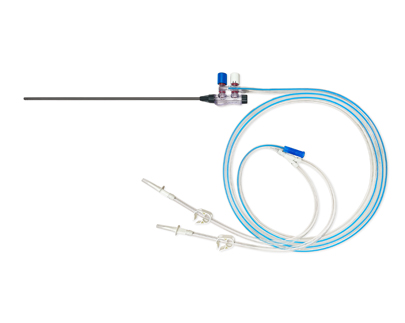
All patients underwent surgery 3-7 days after menstruation was clean, fasted for 8 hours before surgery, placed 1 mg carboprost suppository into the vagina half an hour before surgery to dilate the cervix, and performed hysteroscopy under the detection of B-ultrasound. Uterine adhesion decomposition, hysteroscope produced by Japan olympus company. Control group: simply placed a triangular IUD after infection prevention. Research group: About 2 mL of chitosan was injected into the uterine cavity after intrauterine adhesions, and a balloon uterine stent was placed; the intrauterine adhesions were placed in the uterine cavity, and the balloon catheter was No. 14, according to the operating instructions The balloon is inflated with sterile saline, and the IUD is placed after the balloon is removed 4-5 days after surgery. Both groups of patients were treated with estrogen and progesterone sequential therapy for artificial cycle treatment for 2 months, and underwent hysteroscopy review after 2 months.
1.3 Evaluation indicators
The clinical efficacy, intrauterine re-adhesion 1 month and 2 months after operation, postoperative bleeding volume, menstrual recovery and complications (infection, uterine perforation, massive bleeding) were compared between the two groups. Efficacy evaluation[4]: markedly effective: the menstruation of the patients returned to normal, the dysmenorrhea disappeared, and the hysteroscopy observation was normal, and no adhesion occurred. Effective: The menstrual flow of the patient has increased, the dysmenorrhea is reduced, no adhesion occurs, and one or both uterine horns are not visible in the hysteroscopy review. Invalid: Refers to patients with no change in menstrual flow, no dysmenorrhea, a barrel-shaped uterine cavity, and stenosis or adhesions in the uterine cavity. Total effective rate = apparent rate + effective rate.
1.4 Statistical methods
All the data were counted on SPSS17.0 software, among which the measurement data was represented by (x±s), and the t test was used, and the count data was used the x2 test. 2 Results 2.1 Comparison of clinical efficacy between the two groups It can be seen from Table 1 that the total effective rate of the study group was 91.4% (32/35), which was significantly higher than that of the control group, 77.1% (27/35), and the difference between the two groups was statistically significant (P< 0.05).
2 Discussion
Uterine adhesions were first reported in detail in 1894. Clinically, there are mainly less menstruation, amenorrhea, dysmenorrhea, habitual abortion, and infertility. Later, intrauterine re-adhesion is more likely to occur [5-7]. Surgical procedures involving the uterine cavity, the isthmus, and the uterine tube — especially those requiring instruments such as a uterine manipulator — can increase the chance of infection, which can lead to postoperative adhesions. According to statistics, about 90% of patients with intrauterine adhesions are caused by curettage and curettage. The main factors of intrauterine adhesions are mechanical injury, infection, tissue hypoxia and foreign body stimulation, which leads to the appearance of uterine cavity, abdominal cavity and pelvis adhesion. In addition, long-term peritoneal dialysis, gynecological diseases, and fluid perfusion may also cause pelvic and abdominal adhesions [8-10]. Pregnancy is the main susceptibility factor for intrauterine adhesions. Pregnant patients will cause uterine cavity damage due to miscarriage and termination of pregnancy, and eventually form intrauterine adhesions due to various factors [11].
In recent years, with the increase of spontaneous abortion and induced abortion, the number of intrauterine adhesions has also increased year by year. After intrauterine adhesion separation, the endometrium of the patient needs to be repaired for a long time, but patients are more likely to have intrauterine re-adhesion during the repair period [12-15]. Balloon uterine stent; intrauterine adhesions are mainly composed of silicone stents, and silicone stents are mainly composed of balloons, catheters and catheter holders. The better stent effect can make the inner wall of the uterus press evenly, better prevent uterine bleeding, and then promote the regular growth of the endometrium [16]. The sodium hyaluronate can bind the wound tightly and protect the wound to a certain extent, thereby giving the endometrium a chance to repair, reducing the occurrence of inflammatory reactions, and ultimately preventing the occurrence of re-adhesion[17]. This study found that the total effective rate of the study group was 91.4% (32/35), which was significantly higher than that of the control group, 77.1% (27/35), which was consistent with the results of other studies [18,19], indicating that the balloon uterine stent; Intrauterine adhesions have good clinical efficacy in preventing re-adhesion after intrauterine adhesions, and can significantly improve postoperative conditions. The total adhesion rate in the study group was significantly lower than that in the control group at 1 month and 2 months after operation, and the total postoperative bleeding in the study group was significantly lower than that in the control group, indicating that balloon uterine stents; intrauterine adhesions can significantly reduce the total postoperative adhesions rate, and can significantly reduce postoperative intrauterine bleeding. The final study also found that the total incidence of complications in the study group was significantly lower than that in the control group, and the menstrual recovery rate was significantly higher than that in the control group, which was consistent with the results of other studies [20], indicating that the balloon uterine stent; Intrauterine adhesions can significantly reduce the incidence of postoperative complications and improve the menstrual recovery rate of patients. Analysis of the reasons may be related to the balloon uterine stent; intrauterine adhesions can fill the uterine cavity, thereby compressing the endometrium, and its pressure is relatively uniform, thereby reducing the occurrence of postoperative complications and preventing re-adhesion of the uterine cavity. occurrence, restore the patient's menstruation.
To sum up, intrauterine adhesion is a common disease, which has great harm to patients. Balloon uterine stent; intrauterine adhesion surgery has good clinical efficacy in intrauterine adhesion surgery, and can significantly reduce postoperative bleeding. It can reduce the postoperative re-adhesion rate, and can significantly reduce the occurrence of complications.